Treatments
Minimally invasive surgery For Uterine & Endometrial Cancer
Minimally Invasive Cancer Care with Compassion and Precision
Dr. Lucas Minig – Minimally Invasive Surgery Expert Care in robotic & laparoscopic surgery for endometrial cancer
Request Consultation or Second Opinion

You Deserve Expert Care — Without Delay
A diagnosis of uterine or endometrial cancer can raise urgent questions:
- What stage is it?
- What are my treatment options?
- Will I need to lose my uterus or ovaries?
At our internationally recognized center in Valencia, we offer rapid, personalized surgical care using the latest minimally invasive techniques. Most patients have surgery scheduled within days of their consultation — with compassionate support every step of the way.
DOWNLOAD A FREE Roadmap
FREE Endometrial Cancer Symptom & Diary Kit
Keep track of your daily symptoms, pain levels, and treatment responses with our expert-designed PDF. This tool helps both you and your care team identify patterns and optimize your plan.
What Type of Surgery Is Needed?
Most early-stage uterine and endometrial cancers are treated with laparoscopic or robotic surgery. These modern techniques:
- Avoid large incisions
- Minimize pain and recovery time
- Reduce the risk of complications
In almost all cases, surgery includes:
- Hysterectomy (removal of the uterus and cervix)
- Sentinel lymph node mapping or lymphadenectomy
- Adnexectomy (removal of ovaries and fallopian tubes) in postmenopausal women or selected cases of premenopausal patients
Each decision is tailored to your diagnosis, your age, and your fertility or hormone preservation goals.
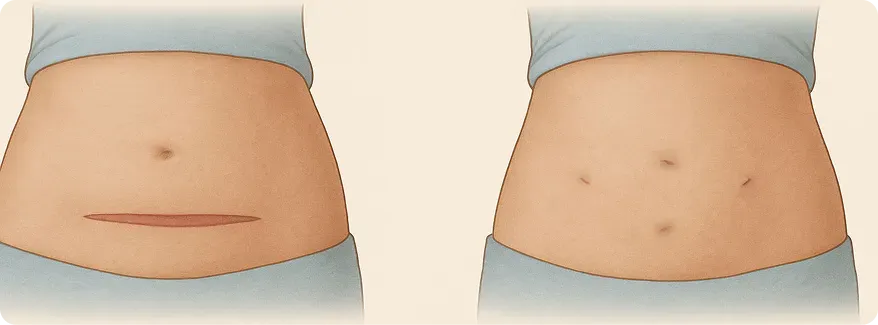
Minimally Invasive Hysterectomy. removes the uterus and cervix through a few small incisions. It is the gold standard for early-stage cancer.
At our clinic, we perform over 95% of these surgeries laparoscopically or with robotic assistance.
Patients from around the world trust our expertise to treat even the most complex cases that local providers may not manage.
Why It Matters:
- Shorter hospital stay (often 24 hours)
- Lower risk of blood loss and infection
We also prioritize nerve-sparing techniques to protect bladder, bowel, and sexual function—especially during radical hysterectomies.
All surgical procedures are performed by Dr. Lucas Minig, a global leader in complex gynecological surgery. Surgeries are performed under general anesthesia using 4 small incisions (5 mm) in the pelvis. The Surgery take over 90 - 120 minutes.
Sentinel Lymph Node Mapping
This technique identifies the first lymph node that may receive cancer cells from the uterus.
By injecting a dye and tracking its path, we often only need to remove 1–3 nodes instead of 20 radical lymph node removal
Benefits:
- Lower risk of swelling (lymphedema) & other complications
- Faster recovery
- More precise staging
Patients from around the world trust our expertise to treat even the most complex cases that local providers may not manage.
Do the Ovaries Always Need to Be Removed?
Not always. For premenopausal women with early-stage disease, we often preserve the ovaries safely—avoiding early menopause and the need for lifelong hormone therapy.
This decision depends on your cancer type and personal risk factors. We discuss it openly with you.
Recovery Timeline
Many of our global patients return home within days of surgery. Your aftercare is supported through virtual check-ins and local care coordination.
Days 0-1
Urinate by yourself. Walking. Hospital dishcarge by Dr Minig in-person
Days 1-15
Progressive home recovery; virtual follow-up. Day 10 - 15: travel to your city/country
Weeks 2–4
Normal activities resume according with level of pain; discomfort fades.Back to work. virtual follow-up.
Months 1–3
Back to full rutine, including work and excercises. virtual follow-up...
Ongoing
Annual ultrasounds help monitor for recurrence
We guide you through every step, with virtual check-ins and personalized aftercare.
When Can I Return to Work?
Most patients return to office work within 2–3 weeks. If your job involves physical labor or long hours on your feet, plan for 4–6 weeks.
Is This Surgery Fertility-Sparing?
For early, select cases in younger women who wish to preserve fertility, we may consider hormonal therapy and careful monitoring in place of immediate hysterectomy. This is rare, but possible with thorough evaluation.
Why choose Dr. Minig & our team
More than a clinic — we are your international partner in healing.
With over 20 years experience treating global patients, we offer personalized surgical care and full logistical support for those traveling to Valencia.
- Specialized Expertise: Dr. Minig is a gynecologic oncologist with advanced training in complex minimally invasive laparoscopic & robotic surgery for endometrial cancer
- Minimally Invasive Excellence: Over 95% of our surgeries utilize laparoscopic or robotic techniques.
- Individualized Care: We align treatment with your pain tolerance, fertility desires, and lifestyle.
- Whole-Woman Approach: From surgery to nutrition and emotional well-being, we support every facet of your health.
- Industry-Leading Research & Innovation
- Global Reach: Personalized logistical support for international patients
“I left the hospital the next day with almost no pain — and no large scar to remind me.”
— Marta S., Valencia

International patient welcome
Whether you’re in Europe, North America, or beyond, our clinic offers:
Tele-Consultations in English, Spanish and Italian
Concierge Travel Assistance for visas, lodging, and local transportation
Flexible Scheduling to accommodate your time zone
Frequently asked questions
What type of surgery is used to treat endometrial cancer?
The most common approach is a minimally invasive total hysterectomy, which removes the uterus and cervix. In certain cases, it may also include removal of the fallopian tubes, ovaries, and nearby lymph nodes, depending on how far the cancer has spread. Dr. Minig performs over 95% of these surgeries laparoscopically—meaning smaller incisions, less pain, and a faster recovery.
Will I need my lymph nodes removed during surgery?
If the cancer has any risk of spreading, sentinel lymph node mapping or pelvic lymphadenectomy is often performed. This helps determine whether cancer cells have
Ready for Relief? Let’s talk.
Whether you want our symptom kit, the patient guide, or to speak directly with Dr. Minig, we’re here for you.