TREATMENTS
Endometriosis Treatment Options and Management
Endometriosis is a chronic medical condition that affects millions of women worldwide, often causing debilitating pain and fertility challenges. While it remains a significant health concern, effective treatments exist to manage symptoms and improve quality of life. This article explores the various treatment options, their effectiveness, and answers common concerns for those living with endometriosis.
Request Consultation or Second Opinion

Individualized Treatment Plans
Since the severity and symptoms of endometriosis vary from person to person, treatment options are highly individualized. Healthcare providers take several factors into account, such as the severity of symptoms, the patient’s age, fertility goals, and personal preferences. Common treatment options include pain management, hormonal therapies, and surgical interventions, all aimed at alleviating symptoms and preventing disease progression.
DOWNLOAD A FREE Roadmap
FREE Endometriosis Symptom & Diary Kit
Keep track of your daily symptoms, pain levels, and treatment responses with our expert-designed PDF. This tool helps both you and your care team identify patterns and optimize your plan.
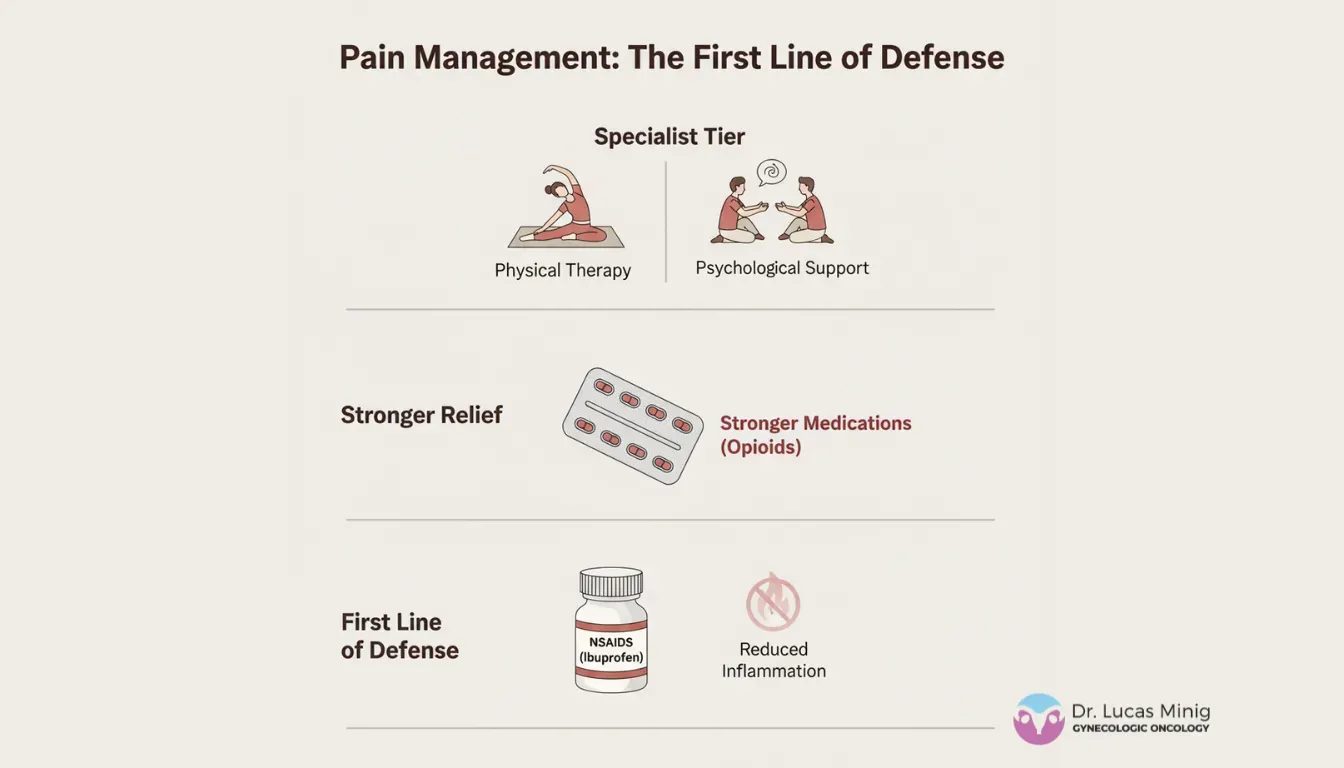
Pain Management: The First Line of Defense
Pain relief is often the first step in managing endometriosis. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen are commonly used to alleviate pain and reduce inflammation. For those experiencing more severe pain, doctors may prescribe stronger medications, including opioids like morphine.
However, for some women, medications may not provide adequate relief. In such cases, specialists may recommend seeing a pain management expert. This could involve additional treatments like physical therapy or psychological support to help manage chronic pain.
Hormonal Therapy: Managing the Root Cause
Hormonal treatments are often used to suppress the growth of endometrial-like tissue and control the menstrual cycle. By regulating or halting the menstrual cycle, these therapies can significantly reduce pain and slow disease progression.
Some common hormonal treatments include:
- Continuous hormonal contraceptives: Available as pills, patches, or vaginal rings.
- Progestins: Either in pill form or through hormonal intrauterine devices.
- GnRH analogs: These drugs lower estrogen levels and effectively stop menstruation.
- Aromatase inhibitors: Often used to reduce the production of estrogen.
While hormonal therapy can be effective, it may come with side effects like weight gain, headaches, hot flashes, and irregular bleeding. For some women, the side effects are manageable, while others may need to explore alternative options.
Surgical Treatment: When It's Necessary
Surgery is typically reserved for severe cases of endometriosis, especially when pain management or hormonal therapy is ineffective. Surgical interventions focus on removing or destroying the endometrial tissue that causes discomfort.
The gold standard for surgical treatment is excision surgery, where the lesions are physically cut out, providing longer-term symptom relief. Alternatively, ablation, which involves burning the tissue, may be performed, though it is less effective and more likely to cause recurrence of symptoms.
For women with endometriosis affecting the uterus, a hysterectomy may be considered. However, it is important to note that while a hysterectomy removes the uterus, it does not guarantee complete pain relief as the extrauterine lesions may still remain. In some cases, surgeons will remove all surrounding tissue during the hysterectomy to ensure a better outcome.
Addressing Fertility Challenges
Fertility can be a concern for many women with endometriosis. While pregnancy is still possible for many, research shows that 30–40% of women with endometriosis may experience difficulty conceiving. Endometriosis-related infertility often occurs due to ovarian cysts or adhesions blocking the fallopian tubes.
Surgical removal of these lesions and adhesions may improve fertility, and in some cases, in vitro fertilization (IVF) can be an option for achieving pregnancy.
It’s important to understand that pregnancy does not cure endometriosis. While some women experience relief from symptoms during pregnancy, the condition often returns after childbirth or when breastfeeding stops.
Lifestyle Changes to Complement Treatment
Along with medical treatments, lifestyle changes can help manage endometriosis symptoms. Regular physical activity, stress management, and a balanced diet may support overall health and improve treatment outcomes.
Women with endometriosis are often encouraged to track their symptoms and monitor any changes with their treatment plan. The timeline for improvement can vary, but many patients notice relief within three to six months of beginning treatment.
Regular Follow-Ups: Maintaining Progress
Regular follow-up appointments are an essential part of managing endometriosis. These appointments help healthcare providers monitor the effectiveness of treatment and make adjustments as necessary. For most patients, follow-ups are typically scheduled every six to twelve months if symptoms are under control.
Why choose Dr. Minig & our team
More than a clinic — we are your international partner in healing.
With over 20 years experience treating global patients, we offer personalized surgical care and full logistical support for those traveling to Valencia.
- Specialized Expertise: Dr. Minig is a gynecologic oncologist with advanced training in complex endometriosis.
- Minimally Invasive Excellence: Over 95% of our surgeries utilize laparoscopic or robotic techniques.
- Individualized Care: We align treatment with your pain tolerance, fertility desires, and lifestyle.
- Whole-Woman Approach: From surgery to nutrition and emotional well-being, we support every facet of your health.
- Industry-Leading Research & Innovation
“Dr. Minig’s expertise let me restart my workouts just two months after surgery—without fear of a bulge returning.”
— Marta S., Valencia

International patient welcome
Whether you’re in Europe, North America, or beyond, our clinic offers:
Tele-Consultations in English, Spanish and Italian
Concierge Travel Assistance for visas, lodging, and local transportation
Flexible Scheduling to accommodate your time zone
Frequently asked questions
What treatments are available for endometriosis?
Treatments are individualized and based on several key factors including the severity of symptoms, the patient's age, whether they wish to become pregnant, and their personal preferences.
From less to more invasive and efficacy, common options include pain medication, hormone therapy, and surgical intervention. Some people also explore alternative or complementary therapies.
Can endometriosis be cured?
Currently, there is no definitive cure for endometriosis before menopause. Thus, treatment mainly focuses on managing symptoms, slowing the disease's progression, and improving quality of life.
How do I know which treatment is right for me?
Your healthcare provider will help you weigh the options by considering your symptoms, overall health, and goals. For example, if you want to get pregnant, some hormonal therapies will not be appropriate because are mainly contraceptive. On the other hand, women with severe alteration of quality of life and complete motherhood, Raga removal, including hysterectomy can be considered a definitive option of treatment.
Will my symptoms return after treatment?
With medical therapies, symptoms often return after treatment is stopped.
While surgery can offer long-term relief, recurrence is possible and depends on the thoroughness of the procedure. For many, progesterone- based hormonal treatments are continued after surgery to reduce the risk of recurrence.
What pain medications are used?
Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are often used for pain and to reduce inflammation. For more severe pain, a doctor may prescribe stronger medication, including morphine
What if medication is not enough?
If pain continues, you may be referred to a pain management specialist who can offer other treatments, such as working with a physiotherapist or psychologist.
How does hormone therapy help?
By suppressing or stopping the menstrual cycle, hormonal treatments can slow the growth of endometrial-like tissue and relieve pain.
What are the different types of hormone therapy?
Options include:
Continuous combined hormonal contraceptives (pills, patches, or vaginal rings).
Progestins only pills (e.g., orally or hormonal intrauterine device).
GnRH (Gonadotropin-releasing hormone) analogues.
Aromatase inhibitors.
What are the side effects?
Side effects can be related to low estrogen levels and may include headaches, irregular bleeding, weight gain, fatigue, and hot flashes. The specific effects vary depending on the treatment and the individual.
Is surgery necessary for everyone with endometriosis?
No. Surgery is considered a second-line treatment, typically for those with severe pain, infertility, or cases where the disease affects other organs such as big ovarian cysts
What is the "gold standard" surgical technique?
Excision surgery (cutting out the lesions) is considered the gold standard for long-term symptom relief. Ablation (burning the surface) is sometimes performed by less experienced surgeons but is less effective.
Does a hysterectomy cure endometriosis?
No. Endometriosis is defined as tissue growth outside the uterus. While a hysterectomy removes the uterus, it does not remove all the extrauterine lesions and does not guarantee complete pain relief.
Therefore, in women with severe impairment in quality of life, if the hysterectomy is performed, it is also very important to remove all perennial implant shown at the time of the surgery.
Can any gynecologist perform surgical treatment of endometriosis?
No, achieve the best quality of care, it highly relevant that surgical treatment are performed by well-trained gynecological surgeons in highly complex surgical procedure, including minimally invasive, laparoscopic or robotic approaches
Can I get pregnant if I have endometriosis?
Yes, many women with endometriosis can get pregnant, but 30–40% may experience difficulty.
Age and ovarian cysts are common reason. Surgery to remove lesions and adhesions may improve fertility outcomes. For some women, in vitro fertilization technique can be an option to achieve pregnancy.
Does pregnancy cure endometriosis?
No. While symptoms may significantly improve during pregnancy for some, they typically return after giving birth and stopping breastfeeding.
What lifestyle changes can help?
Combining lifestyle changes like regular exercise, stress management, and dietary modifications with medical treatment is safe and can enhance effectiveness.
How long until I see improvement?
The timeline for improvement varies, but many treatments begin to show results within three to six months.
Normally, surgical treatment is after six months of permanent treatment without benefits
How often do I need follow-up appointments?
Follow-up frequency depends on your individual condition and how you respond to treatment, but, if the symptoms improve, check-ups are often scheduled every 6 to 12 months.
Ready for Relief? Let’s talk.
Whether you want our symptom kit, the patient guide, or to speak directly with Dr. Minig, we’re here for you.
Learn what it’s like to travel for expert endometriosis care in Valencia.
Hear from real patients who came to Valencia for expert care.
Watch “My Valencia surgery experience”