Treatments
Sentinel Lymph Node Technique for Gynecological Cancer
A Modern & Targeted Approach to Cancer Staging
Dr. Lucas Minig – Minimally Invasive Surgery Expert Care for women with gynecological cancer
Request Consultation or Second Opinion

What Is the Sentinel Node—and Why It Matters
Your lymphatic system plays a crucial role in your immune response. Lymph nodes, small glands connected by delicate ducts, filter waste and track early signs of disease. When cancer is present, it may spread through these channels—first reaching the sentinel node.
The sentinel lymph node is the first node to receive lymphatic drainage from a tumor. If cancer cells spread, they typically arrive here first. Identifying and analyzing this node gives us critical staging information—while sparing you from unnecessary lymph node removal.
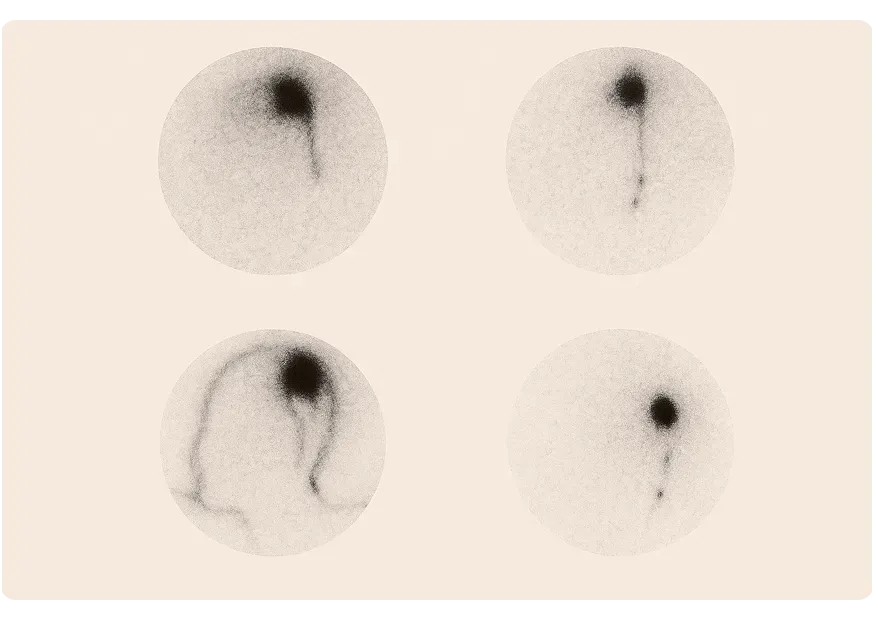
How the Sentinel Node Is Detected
Before surgery, indocianine green, is injected in the uterine cervix. This travel to the lymphatic system, revealing the sentinel node during surgery.
Once identified, the sentinel node is removed and examined by a pathologist. If no cancer is found, there’s no need for full lymph node removal. But if cancer is detected, additional lymphadenectomy may be performed for complete staging.
Benefits of Sentinel Node Mapping
- Minimally invasive: Avoids unnecessary removal of healthy lymph nodes.
- Faster recovery: Less disruption to the lymphatic system.
- Reduced complications: Lower risk of lymphedema, seroma, and nerve damage.
- Precise staging: Helps tailor further treatment like chemotherapy or radiation.
Who Is This Technique For?
Sentinel node detection is now routinely used in:
- Early-stage breast cancer
- Cervical cancer; endometrial cancer, Vulvar cancer
At our center in Valencia, we apply this method with leading-edge tools and a dedicated multidisciplinary team.
Patients from around the world trust our expertise to treat even the most complex cases that local providers may not manage.
What to Expect From the Procedure
- Outpatient or short-stay surgery
- Injection of dye or tracer pre-operatively
- Sentinel node identification and removal
- Immediate pathology review (when needed)
- Clear treatment direction based on your results
Understanding the Risks
When a full lymphadenectomy is performed, potential side effects include:
- Lymphedema: Swelling in the affected limb or area
- Seroma: Fluid accumulation at the surgical site
- Pain or limited mobility
- Increased infection risk
We take every measure to minimize these outcomes, using precision techniques and expert follow-up care.
Why Choose Dr. Minig Individualized Gynecological Cancer Care with Sentinel Node Mapping?
More than a clinic — we are your international partner in healing.
With over 20 years experience treating global patients, we offer personalized surgical care and full logistical support for those traveling to Valencia.
- Specialized Expertise: Specialist in advanced gynecologic surgery
- Minimally Invasive Excellence: Over 95% of our surgeries utilize laparoscopic or robotic techniques.
- Individualized Care: We align treatment with your pain tolerance, fertility desires, and lifestyle.
- Whole-Woman Approach: From surgery to nutrition and emotional well-being, we support every facet of your health.
- Industry-Leading Research & Innovation

International patient welcome
Whether you’re in Europe, North America, or beyond, our clinic offers:
Tele-Consultations in English, Spanish and Italian
Concierge Travel Assistance for visas, lodging, and local transportation
Flexible Scheduling to accommodate your time zone
Frequently asked questions
What are the possible risks of a full lymph node removal (lymphadenectomy)?
While complete lymphadenectomy may be necessary in some cases, it does carry potential risks. These can include:
- Lymphedema: Swelling, often in the legs, caused by disruption to normal lymph flow. This can lead to discomfort, heaviness, or changes in the skin.
- Seroma: Accumulation of lymphatic fluid under the skin near the surgical site, forming a temporary lump or swelling.
- Nerve-related symptoms: Numbness, tingling, or pain due to nerve involvement in the surgical area.
- Reduced mobility: Temporary difficulty moving the affected area post-surgery.
- Increased risk of infection: Due to fluid buildup or wound healing challenges.
These risks are significantly reduced when only the sentinel node is removed, rather than performing a full lymphadenectomy.
Who should perform sentinel node detection and lymphadenectomy?
Sentinel lymph node detection is a highly specialized procedure that should be carried out by a multidisciplinary team:
- Gynecologic oncologist: Leads the surgical intervention.
- Nuclear medicine specialist: Oversees the imaging and injection of tracers.
- Radiologist: Helps localize the sentinel node.
- Pathologist: Performs in-depth analysis of the node during surgery.
This level of collaboration ensures accurate detection, minimizes complications, and improves overall cancer care outcomes.
If you’ve been diagnosed with a gynecologic malignancy, we encourage you to consult with our team in Valencia or book an online consultation from anywhere in Spain to discuss next steps.
What are the benefits of the sentinel node technique?
- Greater precision: The sentinel node—the first node likely to receive cancer cells—is examined with enhanced detail, allowing for the detection of even microscopic metastases.
- Fewer complications: Because only one or a few lymph nodes are removed, there’s a lower risk of surgical side effects like lymphedema or infection.
- Better quality of life: Patients often recover faster, with fewer limitations and better long-term outcomes.
This technique allows us to stage cancer more accurately while preserving your well-being as much as possible.
Ready for Relief? Let’s talk.
Whether you want our symptom kit, the patient guide, or to speak directly with Dr. Minig, we’re here for you.