Learn how to prevent endometrial cancer with evidence-backed lifestyle and medical tips. Expert guidance from Dr. Lucas Minig — book a fast video consult in Spain.
Introduction
Endometrial cancer is one of the most common gynecologic cancers, yet in many cases it is also one of the most preventable. Understanding how to prevent endometrial cancer starts with knowing the risk factors, recognizing early warning signs, and taking evidence-based steps to protect uterine health.
This guide explains what endometrial cancer is, who is most at risk, and how lifestyle choices, medical care, and early evaluation—especially within the healthcare system in Spain—can significantly reduce risk. With clear, practical guidance and insights from experienced gynecologic specialists such as Dr. Lucas Minig, this content is designed to help women make informed, proactive decisions about their long-term health.
Table of Contents
What is endometrial cancer?
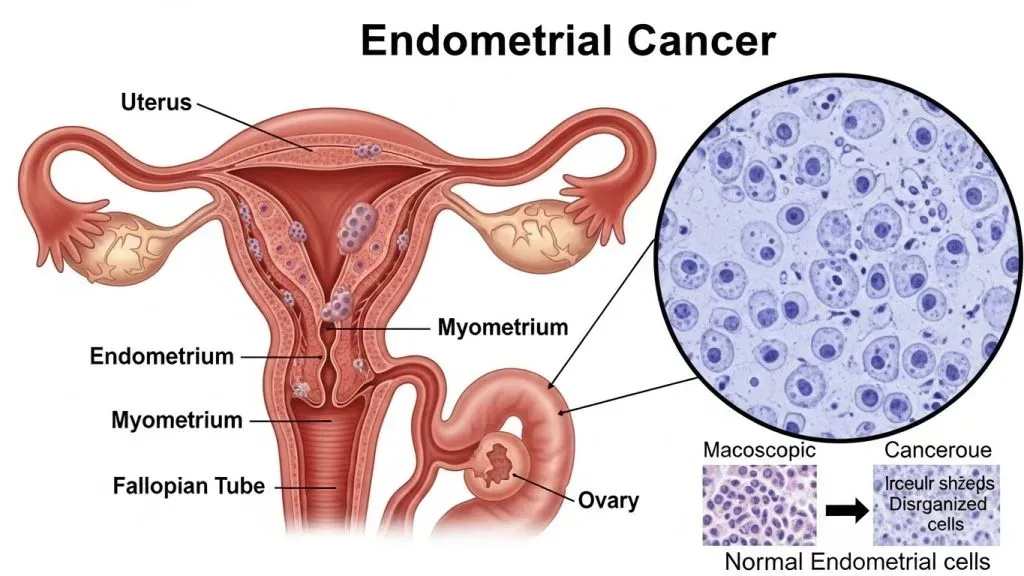
Endometrial cancer — often referred to as uterine cancer when speaking broadly — develops in the lining of the uterus called the endometrium. It typically starts as abnormal growth of the cells that line the uterus and, if unchecked, can invade deeper tissues or spread. Why should you care? Because this is one of the gynecologic cancers most often detected early: abnormal bleeding prompts evaluation, and early-stage disease is highly treatable. But prevention matters: many of the strongest risk factors are modifiable, and a few well-timed clinical actions can dramatically reduce your chance of developing the disease.
In plain language: endometrial cancer = cancer of the uterine lining. It’s important because it tends to present with symptoms early (especially bleeding), and because lifestyle and medical choices influence risk. Think of the endometrium like a garden bed — if the soil conditions (hormone balance, inflammation, metabolic health) are wrong, abnormal growths are more likely. The good news? You can improve the soil.
Types of endometrial (uterine) cancer
Clinicians commonly categorize endometrial cancers into patterns based on behavior and underlying biology. The two practical groups to understand are:
- Type I (estrogen-related): the most common, often slower-growing and linked to prolonged estrogen exposure (unopposed estrogen). These are the “garden bed” cancers affected by metabolic health and hormonal balance.
- Type II (non–estrogen related): less common, more aggressive, and not clearly tied to hormonal risk factors. These behave differently and require distinct clinical attention.
Both types need prompt diagnosis, but prevention strategies are more effective for Type I cancers because they address modifiable hormonal and metabolic drivers.
Common symptoms: abnormal bleeding and more
The hallmark symptom of endometrial cancer is abnormal uterine bleeding. That includes:
- Any bleeding after menopause (this is always concerning).
- Spotting or bleeding between periods in premenopausal women.
- Heavier-than-usual menstrual bleeding that is new and persistent.
Other possible symptoms: unusual vaginal discharge, persistent pelvic pain, or unexplained weight loss. If you notice any of these, do not ignore them — early evaluation saves more than anxiety; it can save a life.
Who is most at risk? — Key risk factors
Understanding risk helps you prioritize prevention. Some factors you cannot change (age, genetics), but many you can (weight, metabolic control, hormone choices).
Age and menopausal status
Endometrial cancer is most common in women after menopause. The median age at diagnosis tends to be in the 60s in many populations. That doesn’t mean younger women are immune, but your risk increases with age, particularly when other risk factors accumulate.
Obesity and metabolic syndrome
Excess body fat is one of the strongest, modifiable risk factors. Fat tissue converts adrenal and ovarian androgens into estrogens — increasing lifetime estrogen exposure and stimulating the endometrium. Metabolic syndrome (high blood pressure, high blood sugar, abnormal lipids, central obesity) compounds the risk. In practice: reducing body fat and improving metabolic health reduces hormone-driven stimulation of the endometrium.
Diabetes and insulin resistance
Independent of weight, diabetes and insulin resistance increase risk. Insulin and insulin-like growth factors can promote cell proliferation. Good glucose control — through diet, exercise, and medication when necessary — is a cancer-preventive action as well as a diabetes management goal.
PCOS, infertility, and prolonged estrogen exposure
Polycystic ovary syndrome (PCOS) and other causes of chronic anovulation mean prolonged or unopposed estrogen exposure — no ovulatory progesterone to counterbalance estrogen’s effect on the endometrium. Women with long-standing irregular cycles or infertility should be monitored and, when indicated, treated to regulate cycles.
Genetic risk: Lynch syndrome and family history
Lynch syndrome (hereditary nonpolyposis colorectal cancer) markedly increases the risk of endometrial cancer. If you have close relatives with colorectal, endometrial, ovarian, or related cancers, ask about genetic counseling. For mutation carriers, targeted surveillance or even risk-reduction strategies may be recommended.
Primary prevention strategies: Evidence-based actions
Prevention is layered: lifestyle measures, medical choices, and targeted clinical surveillance for those at higher genetic or clinical risk.
Maintain a healthy weight — why this matters
Reducing weight by even 5–10% improves hormone balance and insulin sensitivity. It’s not about perfection — small, sustained losses reduce the biological drivers of Type I endometrial cancer. Practical tactics include portion control, replacing sugary drinks, and consistent physical activity. Think of weight loss as soil improvement for that garden bed.
Move more: physical activity guidelines
Aim for at least 150 minutes per week of moderate-intensity aerobic activity (walking, cycling, brisk swimming) or 75 minutes of vigorous activity plus twice-weekly strength training. Physical activity lowers insulin levels, reduces inflammation, and helps manage body weight — all protective mechanisms against endometrial cancer.
Dietary habits that support uterine health
A Mediterranean-style diet — vegetables, fruits, legumes, whole grains, fish, olive oil, and nuts — supports metabolic health and reduces inflammatory markers. Limit processed foods, refined sugars, and excessive processed red meats. Small, consistent dietary improvements pay off over years.
Control diabetes and metabolic risk
If you have prediabetes or diabetes, working with primary care and endocrinology to achieve glycemic targets is prevention. Lifestyle (diet, exercise) plus medications like metformin when indicated improve insulin sensitivity and may reduce cancer risk. Regular monitoring and treatment of hypertension and dyslipidemia also make a difference for overall cancer and cardiovascular outcomes.
Manage PCOS and irregular cycles
Managing PCOS often involves hormonal regulation: combined hormonal contraception or cyclic progestins (or a levonorgestrel-releasing IUD) reduce unopposed estrogen exposure to the endometrium. Weight loss and insulin-sensitizing treatments help too. If you have prolonged irregular bleeding, talk to your doctor — it’s not just cosmetic, it’s preventive.
Reproductive factors and protective effects (OCP, pregnancy, breastfeeding)
Epidemiological data show that long-term use of combined oral contraceptives (OCPs) and having had full-term pregnancies reduce endometrial cancer risk. Breastfeeding may add modest protection. These are not “treatments” for everyone but explain part of why lifetime risk differs between women.
Medical prevention and clinical measures
Some interventions are clinical rather than lifestyle — these require medical supervision.
Hormone therapy: safe approaches in Spain
For symptomatic menopausal women with an intact uterus, combined estrogen–progestogen therapy is safer than estrogen alone because progesterone opposes endometrial proliferation. A progestogen-releasing IUD is an option for local progestin delivery. Always discuss individualized risks and benefits with your gynecologist; dosing, duration, and monitoring matter.
When and why to consider surveillance (high-risk women)
If you have Lynch syndrome, a strong family history, or persistent abnormal bleeding, clinicians may recommend tailored surveillance — periodic transvaginal ultrasounds or endometrial sampling. Surveillance isn’t a population screening tool; it’s for selected higher-risk groups and must be individualized.
Role of genetic testing (Lynch syndrome)
Genetic counseling and testing clarify risk for you and family members. For carriers, options include increased surveillance, prophylactic surgeries after childbearing, or other individualized prevention strategies. Genetic testing is not trivial — counseling is essential before and after testing.
Vaccines and screening: what’s available and what’s not
There is no routine population screening for endometrial cancer (unlike cervical cancer). No vaccine prevents endometrial cancer specifically. Early detection rests on symptom awareness and targeted surveillance of high-risk individuals.
Recognize warning signs early — symptoms you should never ignore
Prevention includes vigilance. Recognizing and acting on early symptoms enables diagnosis at a stage when treatment is simple and outcomes are excellent.
Postmenopausal bleeding and abnormal spotting
Bleeding after menopause should prompt immediate medical evaluation. In premenopausal women, new persistent heavy bleeding or spotting between cycles also needs evaluation. Don’t assume it’s “normal” — many benign conditions cause bleeding, but ruling out endometrial pathology is essential.
Pelvic pain, discharge, and other red flags
Persistent pelvic pain, a change in vaginal discharge (especially if unusual, malodorous, or accompanied by bleeding), or systemic signs like unexplained weight loss deserve assessment. Even when the likelihood of cancer is low, diagnostic steps are straightforward and quick.
How doctors in Spain diagnose and manage early disease?
Spanish public and private systems use standard pathways that allow rapid diagnosis when symptoms appear.
Typical diagnostic steps: ultrasound, biopsy, hysteroscopy
First-line evaluation typically includes a clinical exam and transvaginal ultrasound to measure endometrial thickness. If suspicious, the next step is endometrial sampling (biopsy) or diagnostic hysteroscopy with directed biopsy. These procedures provide definitive tissue diagnosis.
Minimally invasive options and surgical care (role of gynecologic oncologists like Dr. Lucas Minig)
When treatment is required, minimally invasive surgery (laparoscopy or robotic-assisted techniques) is often preferred because it reduces pain, shortens hospital stay, and speeds recovery. Specialists such as Dr. Lucas Minig focus on minimally invasive approaches for early-stage disease and complex cases alike. For many patients in Spain, that means quicker return to daily life and lower perioperative risk. Dr. Lucas and his team also emphasize clear communication: what to expect before, during, and after procedures — and how to combine surgical care with fertility-preserving options when appropriate.
How Dr. Lucas Minig (and doctors in Spain) approach prevention and patient education
Preventive medicine and patient education are as important as surgical skill. In clinics across Spain, including private specialist services, prevention is integrated into routine care.
Counseling, personalized risk assessment, and follow-up
A good clinic begins with conversation: assessing your personal risk (age, BMI, family history, menstrual history, metabolic health), explaining what the risk means, and offering a tailored plan. Dr. Lucas typically discusses lifestyle steps, appropriate medical options (HRT decisions, OCPs, progestin therapy), and when surveillance is warranted. Follow-up is structured: periodic reviews, clear instructions on symptoms to watch for, and easy access to the team if new concerns arise.
Multidisciplinary care and patient support services
Endometrial cancer prevention and care benefit from a team approach — gynecologists, endocrinologists, genetic counselors, dietitians, and physiotherapists. Dr. Lucas’s practice coordinates this multidisciplinary care, offering second opinions, genetic referrals when necessary, and practical support for international patients (travel planning, fast-track appointments). That coordination reduces delays and improves patient confidence and outcomes.
Lifestyle checklist: 10 practical steps to lower your risk
Daily actions, weekly habits, yearly health checks
- Walk briskly 30 minutes most days (or equivalent activity).
- Replace sugary drinks with water or unsweetened tea.
- Add one vegetable to every meal; aim for colorful plates.
- Do resistance training twice weekly (bodyweight or light weights).
- Track portions; small, consistent reductions beat yo-yo dieting.
- If diabetic or prediabetic, aim for stable blood sugars and scheduled medical reviews.
- Maintain regular gynecologic follow-up—report abnormal bleeding promptly.
- Discuss HRT or contraceptive options with your gynecologist to ensure endometrial protection if needed.
- If you have PCOS, follow a plan to regulate cycles (medical and lifestyle interventions).
- Review family history periodically; consider genetic counseling if patterns suggest Lynch syndrome.
How to make prevention realistic — plans for busy people?
Prevention must fit your life. Small changes that you can sustain beat dramatic short-term fixes.
Small wins: micro-habits that compound
Can you swap one sugary snack a day for fruit? Park slightly further and add a 10-minute walk? Micro-habits accumulate. Think of prevention as compound interest: small repeated deposits (walks, healthy meals) yield significant returns over time.
When to ask your doctor for help (telemedicine & second opinions in Spain)
If you’re unsure about symptoms, or you want a personalized prevention plan without long waiting lists, telemedicine is practical. Many specialists in Spain, including Dr. Lucas’s team, offer video consultations and second opinions to review risk factors, imaging, or biopsy results. That allows fast decision-making and guidance on whether in-person evaluation is needed.
FAQ’s
What is the single most effective action I can take to lower my risk of endometrial cancer?
Losing excess weight and improving metabolic health is the most impactful modifiable step. Even modest weight loss improves hormone balance and insulin sensitivity.
Do I need screening if I have no symptoms?
There is no routine population screening for endometrial cancer. Screening is reserved for selected high-risk groups; otherwise, symptom awareness (especially postmenopausal bleeding) guides evaluation.
Can hormonal contraception protect me?
Yes — combined oral contraceptives reduce endometrial cancer risk with long-lasting protective effects. Discuss suitability and options with your gynecologist.
If my mother had endometrial cancer, should I get genetic testing?
A family history that includes multiple early cancers or patterns consistent with Lynch syndrome warrants referral to genetic counseling. The counselor will determine if testing is appropriate.
How quickly should I see a doctor for postmenopausal bleeding?
Seek medical evaluation promptly — within days to a couple of weeks. In Spain, many clinics provide rapid assessment pathways; a quick consultation often leads to ultrasound and, if needed, biopsy to rule out pathology.
Conclusion
Endometrial cancer prevention is realistic and actionable. Focus on what you can change — weight, activity, diet, glucose control, and menstrual health — and pair these with sensible clinical measures: appropriate hormone management, surveillance for high-risk women, and prompt evaluation of symptoms.
In Spain, both public and private practices provide effective diagnostic and treatment pathways; specialist teams — including experienced gynecologic oncologists such as Dr. Lucas Minig — offer streamlined pathways for prevention, diagnosis, and minimally invasive care. Start with one small change this week; that change compounded over months can substantially lower your risk.