DISEASES
Genital Prolapse: Causes, Symptoms, and Treatments
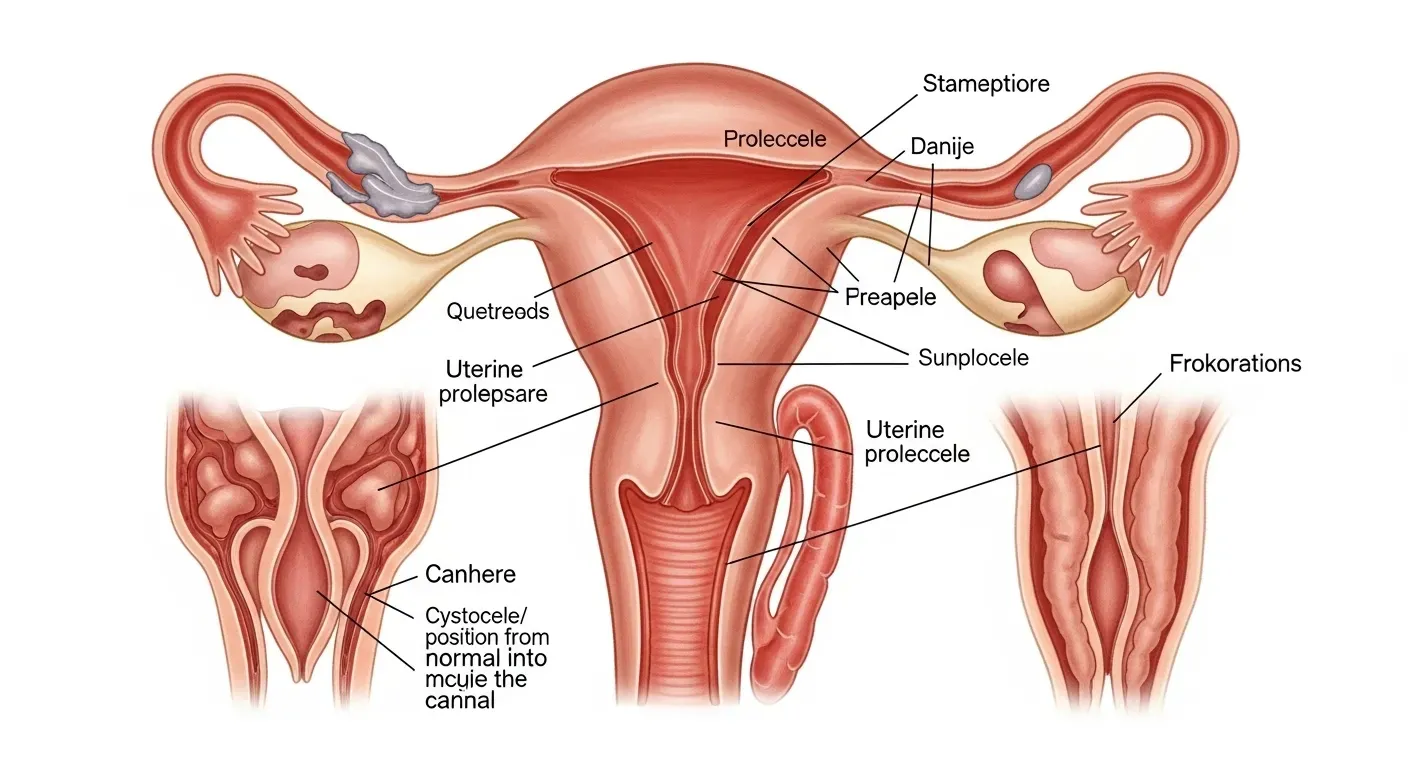
Genital prolapse, also known as pelvic organ prolapse (POP), occurs when the pelvic floor muscles and tissues weaken, causing pelvic organs like the bladder, uterus, and rectum to descend and bulge through the vaginal wall. This condition can range from mild to severe and can significantly affect quality of life.
Request Consultation or Second Opinion

Types of Pelvic Organ Prolapse
Pelvic organ prolapse can involve several organs within the pelvic region, each causing distinct symptoms:
- Bladder Prolapse (Cystocele): The bladder bulges into the front wall of the vagina, often leading to urinary issues.
- Rectal Prolapse (Rectocele): The rectum pushes into the back wall of the vagina, sometimes causing bowel problems.
- Uterine Prolapse: The uterus descends into the vaginal canal, which can cause a sensation of fullness or pressure.
DOWNLOAD A FREE Roadmap
FREE Endometriosis Symptom & Diary Kit
Keep track of your daily symptoms, pain levels, and treatment responses with our expert-designed PDF. This tool helps both you and your care team identify patterns and optimize your plan.
Prevalence of Pelvic Organ Prolapse
This condition is most common in women who have undergone vaginal childbirth, are experiencing menopause, or have been dealing with chronic strain like coughing or heavy lifting. Prolapse may also be more frequent in individuals who are overweight. Though mild cases might not cause noticeable symptoms, more severe cases can significantly disrupt daily activities.
Symptoms of Genital Prolapse
Common symptoms of pelvic organ prolapse include:
- Heaviness or bulging in the vaginal area.
- A sensation of something "falling out" or the feeling of sitting on a ball.
Other possible symptoms include:
- Urinary issues, such as incontinence or difficulty fully emptying the bladder.
- Bowel problems, like constipation or the need to assist bowel movements with fingers.
- Pain or discomfort during sexual intercourse, which may occur in some cases.
Impact on Bladder and Bowel Function
Pelvic organ prolapse can interfere with bladder and bowel functions, often leading to issues such as:
- Urine leakage or difficulty controlling urination.
- Constipation and the need for additional effort during bowel movements.
These symptoms can cause significant discomfort and distress for those affected.
Causes of Weakening Pelvic Floor Muscles
Several factors can contribute to the weakening of the pelvic floor muscles, leading to prolapse. The most common causes include:
- Pregnancy and childbirth, especially vaginal deliveries, which put strain on the pelvic floor.
- Aging and menopause, which result in decreased muscle tone and hormonal changes.
- Physical strain, such as lifting heavy objects, chronic constipation, or long-term coughing.
- Obesity, which puts added pressure on the pelvic region.
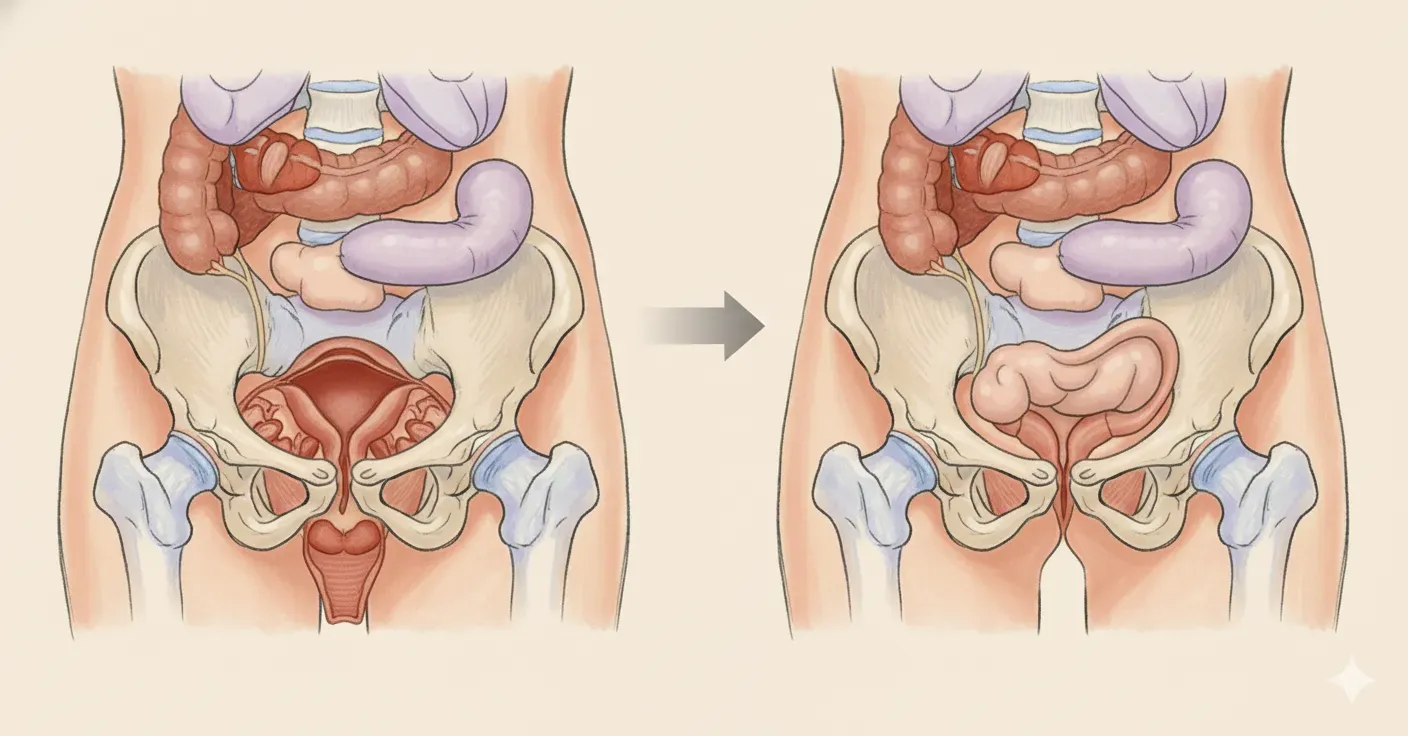
Impact of Hysterectomy on Prolapse
Some women report developing pelvic organ prolapse after undergoing a hysterectomy, especially if the surgery was performed vaginally for pre-existing prolapse. However, research suggests that hysterectomy performed for other reasons does not inherently increase the risk of prolapse.
Surgical Considerations and Recovery
For those who require surgery, recovery times are generally quick, especially with vaginal approaches. While pain after surgery is usually minimal, it is essential to discuss potential side effects, such as discomfort during intercourse or the possibility of prolapse recurrence.
Prognosis and Progression
Prolapse can worsen over time if left untreated, particularly in symptomatic cases. However, mild cases often do not progress, and many individuals can manage symptoms effectively with treatment. Early assessment and regular follow-ups can prevent complications and provide appropriate interventions.
Sexual Activity and Prolapse
For many individuals, sexual activity remains unaffected by prolapse, and intercourse is not likely to cause damage. However, some may experience discomfort or pain, which can often be alleviated with proper treatment. After vaginal surgeries, sexual abstinence is typically recommended for six weeks to allow for healing.
Seeking Help for Pelvic Organ Prolapse
If you suspect you have pelvic organ prolapse, consulting a healthcare provider is crucial. A general practitioner (GP) can evaluate your symptoms and, if necessary, refer you to a specialist such as a urogynecologist, who focuses on pelvic health. Diagnosis usually involves a physical exam and may include additional tests to assess the extent of prolapse.
Why choose Dr. Minig & our team
More than a clinic — we are your international partner in healing.
With over 20 years experience treating global patients, we offer personalized surgical care and full logistical support for those traveling to Valencia.
- Specialized Expertise: Dr. Minig is a gynecologic oncologist with advanced training in complex endometriosis.
- Minimally Invasive Excellence: Over 95% of our surgeries utilize laparoscopic or robotic techniques.
- Individualized Care: We align treatment with your pain tolerance, fertility desires, and lifestyle.
- Whole-Woman Approach: From surgery to nutrition and emotional well-being, we support every facet of your health.
- Industry-Leading Research & Innovation
“Dr. Minig’s expertise let me restart my workouts just two months after surgery—without fear of a bulge returning.”
— Marta S., Valencia

International patient welcome
Whether you’re in Europe, North America, or beyond, our clinic offers:
Tele-Consultations in English, Spanish and Italian
Concierge Travel Assistance for visas, lodging, and local transportation
Flexible Scheduling to accommodate your time zone
Frequently asked questions
What is genital prolapse?
Genital or pelvic organ prolapse (POP) occurs when the pelvic floor muscles and tissues weaken, causing one or more pelvic organs. It can involve the uterus, bladder and / or the rectum. Theses organs descend and bulge through the vagina.
What are the different types?
Common types of prolapse include:
- Cystocele: The bladder bulges into the front (anterior) wall of the vagina.
- Rectocele: The rectum bulges into the back (posterior) wall of the vagina.
- Uterine prolapse: The uterus sags down into the vagina.
Is it common?
Yes, prolapse is common, particularly in women who have given birth, overweight, with chronic cough, and during menopause. A mild prolapse is often asymptomatic and doesn't require treatment.
What does prolapse feel like?
Common symptoms include:
A feeling of a bulge, heaviness, or pressure in the vagina.
A sensation that something is "falling out" or that you are "sitting on a ball."Does it affect bladder and bowel function?
Yes, prolapse can lead to a range of bladder and bowel issues, such as:
Leaking urine (incontinence).
Difficulty starting urination or emptying the bladder completely.
Constipation or straining during bowel movements.
Needing to use your fingers to empty your bowels.Does it cause pain?
It’s a rare symptom, but when occur is especially low back pain or discomfort during sexual intercourse.
What causes the pelvic floor to weaken?
The most common causes are:
Pregnancy and childbirth, especially vaginal births.
Menopause and aging, which lead to decreased muscle tone.
Physical strain from heavy lifting, chronic constipation, or a long-term cough.
Being overweight or obese.Does having a hysterectomy cause prolapse?
Some women report developing prolapse after a hysterectomy, particularly if it was performed vaginally for a pre-existing prolapse. However, clinical studies fail to demonstrate that performing hysterectomy by other reasons, is associated with an increased risk of genial prolapse.
What are the non-surgical options?
Treatments vary depending on the severity of the prolapse and may include:
- Kegel exercises: Strengthening the pelvic floor muscles can reduce symptoms.
- Vaginal pessary: A removable silicone device inserted into the vagina to provide support for the pelvic organs.
- Lifestyle changes: Losing weight, avoiding heavy lifting, and preventing constipation can help manage symptoms.
When is surgery needed?
A doctor will recommend surgery if previous treatments are ineffective or the prolapse is more severe. Options include repairs to tighten the vaginal walls or procedures to address multiple prolapse compartments.
What is the recovery like after surgery?
Recovery time and potential side effects, like pain during intercourse or a recurrence of prolapse, should be discussed with a doctor. However, usually are surgeries performed through vaginal route with fast recovery and low level of pain after surgery
Can prolapse get worse?
Will it progress if left untreated? An untreated prolapse may worsen over time, especially if a patient is symptomatic. Mild cases may not progress, but an early assessment and close follow-up of progression is recommended.
Does prolapse affect sexual activity?
Is it safe to have sex with a prolapse? Yes. Intercourse will not cause damage, and for most women, a prolapse is not noticeable during sex. Some women may experience pain or discomfort, which can be improved with treatment.
Sexual abstinence is recommended for the following six weeks after vaginal procedures.
Who should I see?
A general practitioner can provide an initial assessment, but they may refer you to a specialist like a urogynecologist, who focuses on female pelvic health.
How is it diagnosed?
A healthcare provider will discuss your medical history and symptoms, perform a physical exam, and may order additional tests.
Ready for Relief? Let’s talk.
Whether you want our symptom kit, the patient guide, or to speak directly with Dr. Minig, we’re here for you.
Learn what it’s like to travel for expert endometriosis care in Valencia.
Hear from real patients who came to Valencia for expert care.
Watch “My Valencia surgery experience”