DISEASES
Multidisciplinary Endometrial Cancer Care in Valencia
Multidisciplinary Rapid Diagnosis & Personalized Minimally Invasive Treatment — Trusted by Women Worldwide
Dr. Lucas Minig — Expert Gynecologic Oncology & Fertility-Sparing Care

You Deserve Answers—and Action—Today
Any unexpected bleeding—spotting between periods, bleeding after intercourse, or post-menopausal bleeding—warrants prompt evaluation. These can be early warning signs of endometrial cancer. Catching it sooner expands your treatment options and often reduces the need for more aggressive therapy.
At our Valencia center, Dr. Minig and his expert team deliver accelerated work-ups—imaging, biopsy, and staging—all within days.
Our mission: craft a clear, personalized treatment plan that maximizes cancer control while preserving your well-being and future choices, offering world-class surgical outcomes with a truly human approach.
DOWNLOAD A FREE Roadmap
FREE Endometrial Cancer Roadmap (PDF)
Screening & staging timelines
- Surgical, hormonal & radiation options
- FAQs on fertility preservation, side effects & follow-up
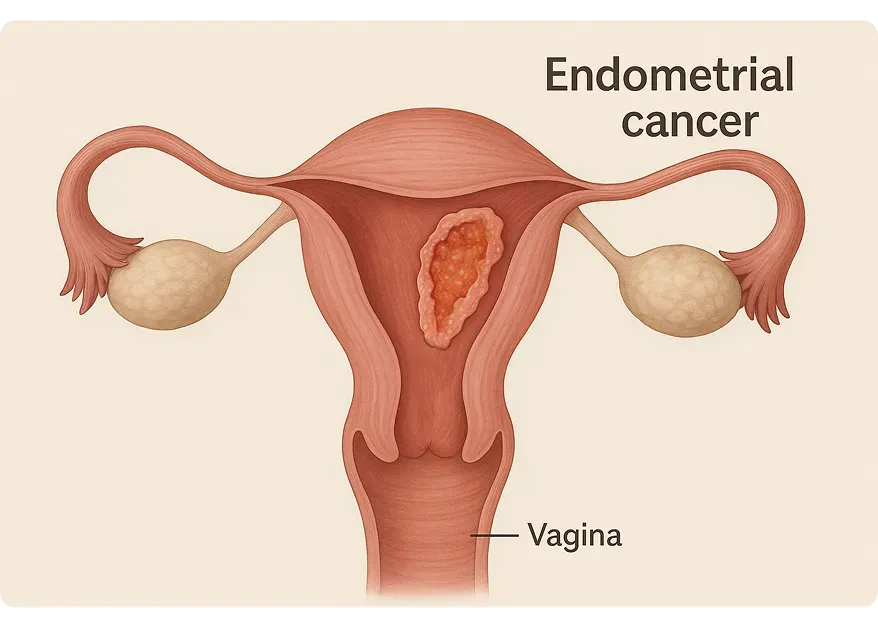
What Is Endometrial Cancer?
Endometrial cancer arises when the inner lining of the uterus (endometrium) develops malignant cells. Because symptoms often appear early, timely evaluation can halt progression before invasive spread occurs—improving outcomes and preserving fertility when possible.
Patients worldwide trust our minimally invasive approach (laparoscopic or robotic surgery) to treat both early-stage and advanced disease.
Early Warning Signs
Catching symptoms early can radically shift your outcome. Here are signs to pay attention to.
Post-Menopausal Bleeding
Any persistent bleeding after menopause should be assessed. Even a small amount matters.
Bleeding Between Periods (Intermenstrual Bleeding)
Unexpected bleeding outside your cycle can indicate a hormonal shift or something more. It’s worth tracking and discussing.
Pelvic Pain or Pressure
Ongoing pelvic discomfort, heaviness, or pain during sex may be subtle but persistent. Don’t dismiss recurring sensations.
Unusual Vaginal Discharge
A sudden change in color, texture, or odor—especially if persistent—could point to infection or underlying inflammation.
Urinary or Bowel Changes
Needing to urinate more often, constipation, or pressure in the bladder or rectum may suggest deeper pelvic involvement.
Who’s at Risk & Why It Happens
Understanding your personal risk empowers better screening, earlier detection, and proactive care.
Most cases occur after menopause. As estrogen levels shift and immune surveillance weakens with age, abnormal cell growth becomes more likely.
Obesity & Metabolic Syndrome
Excess fat tissue produces estrogen, which can overstimulate the endometrial lining. Insulin resistance and chronic inflammation also play a role in tumor development.
Diabetes & High Blood Pressure
These conditions don’t just affect the heart. They alter blood flow and cellular repair mechanisms, creating an environment where abnormal cells are more likely to grow.
Unopposed Estrogen Therapy
Using estrogen without progesterone—especially in women with a uterus—can thicken the endometrial lining over time, increasing cancer risk.
Tamoxifen Use
This breast cancer treatment acts as an estrogen blocker in the breast but can stimulate estrogen receptors in the uterus, making long-term use a risk factor.
Family History & Genetics
A strong family history of endometrial or colon cancer—especially with known Lynch syndrome—greatly increases risk. Carriers of Lynch mutations can face up to a 70% lifetime chance.
How We Diagnose & Stage—Efficiently
When something feels off, getting clear answers—quickly and compassionately—matters. Our diagnostic process is designed to be as precise and minimally invasive as possible, with your comfort and clarity in mind.
- Transvaginal Ultrasound
This is often the first step. It’s a simple imaging test that looks at the uterus from the inside, measuring the endometrial lining and checking for any unusual growths. It’s non-invasive and can offer immediate insight. - Endometrial Biopsy
If needed, a small sample of tissue is gently taken from the uterine lining right in the office. The procedure is brief and helps determine whether any abnormal cells are present. You’ll be supported every step of the way. - MRI or CT Scan
These scans give us a fuller picture—showing whether anything has spread beyond the uterus. They’re safe, non-invasive, and help guide the best treatment approach. - Staging Laparoscopy or Robotic Surgery (Minimally Invasive)
In most cases, we may recommend a minimally invasive procedure to see inside the abdomen. Through tiny incisions, we are able to remove the uterus and ovaries, and we can also assess sentinel lymph nodes and take washings. This approach often avoids more invasive surgeries and helps speed up recovery.
Request Consultation or Second Opinion

Your personalized & multidisciplinary treatment pathway
We personalize every step — whether you are local or traveling from overseas.
Our team coordinates closely with international patients to minimize travel stays and ensure fast, streamlined care.
No two people — and no two diagnoses — are exactly the same. That’s why we take the time to understand your stage, your goals, and your vision for the future, including fertility and quality of life. You are not a case—you are a person. And your care plan will reflect that.
1. Surgical Management
For most, surgery is the first and most effective step. We prioritize techniques that are both thorough and as gentle on your body as possible.
- Total Laparoscopic Hysterectomy with Bilateral Salpingo-Oophorectomy
Removal of the uterus, fallopian tubes, and ovaries—done through small incisions to reduce recovery time and preserve body integrity. - Sentinel Lymph Node Mapping
A targeted approach that helps avoid full lymph node dissection unless necessary—minimizing long-term complications like swelling or pain. - Aortic & Pelvic Lymphadenectomy
Performed only when truly needed, to ensure accurate staging in higher-risk cases. - Omentectomy for High-Risk Histologies
If certain aggressive cancer types are present, we remove the membrane covering the abdomen to reduce spread risk.
“Over 95% of our patients’ surgeries are minimally invasive—smaller scars, less pain, faster recovery, and a quicker return to your life.”
2. Adjuvant Therapies
After surgery, some people may need additional treatment to prevent recurrence. These decisions are personalized and made together.
- Radiation Therapy
External beam or internal (brachytherapy), depending on risk level. It’s focused, precise, and often well-tolerated. - Chemotherapy
Recommended for more advanced stages or aggressive subtypes. We walk with you through every cycle, offering full support. - Hormonal Therapy
In some low-grade cases, hormone-blocking treatments can slow or stop cancer growth with fewer side effects.
3. Fertility-Sparing Options
For those who wish to become pregnant in the future, we listen carefully and proceed with compassion.
- High-Dose Progestin Therapy – Intrauterine Device (IUD)
Medications that suppress abnormal growth while preserving the uterus—closely monitored with regular imaging and biopsies. - Trachelectomy, Tumor Resection + Hormonal Management
For very select cases, this approach carefully removes localized tumors while protecting fertility.
“If motherhood is part of your vision, we’ll explore every evidence-based option to support that dream.”
DOWNLOAD A FREE Roadmap
Download the Endometrial Cancer Roadmap (PDF)
Recovery Timeline after surgery: What to Expect
Many of our global patients return home quickly, supported by virtual check-ins and local coordination.
Days 0-1
Urinate by yourself. Walking. Hospital dishcarge by Dr Minig in-person
Days 1-15
Progressive home recovery; virtual follow-up. Day 10 - 15: travel to your city/country
Weeks 2–4
Normal activities resume according with level of pain; discomfort fades.Back to work. virtual follow-up.
Months 1–3
Back to full rutine, including work and excercises. virtual follow-up...
Ongoing
Annual ultrasounds help monitor for recurrence
Lifestyle & Wellness Support
- Anti-Inflammatory Nutrition: Olive oil, leafy greens, fatty fish; limit processed sugars
- Safe Exercise Plan: Gentle yoga, walking, pelvic-floor rehab
- Emotional Care: Counseling, support groups, mindfulness practices
- Bone Health: Calcium, vitamin D, weight-bearing activities post-oophorectomy
Small, consistent habits enhance recovery and long-term health.
Why choose Dr. Minig & our team
Extensive specialized oncology training in the main medical centers in Italy and the United States
- Rapid, Coordinated Care: Tests and therapies start within days
- Minimally Invasive Expertise: Over 95% of surgeries via laparoscopy/robotic approach
- Multidisciplinary Collaboration: Gynecologic oncology, radiation, pathology, nutrition & psycho-oncology
- Customized Plans: Aligned with your stage, health profile & life goals
- Industry-Leading Research & Innovation
- Global Reach: Personalized logistical support for international patients
“Dr. Minig’s expertise let me restart my workouts just two months after surgery—without fear of a bulge returning.”
— Marta S., Valencia

International patient welcome
Whether you’re in Europe, North America, or beyond, our clinic offers:
Tele-Consultations in English, Spanish and Italian
Concierge Travel Assistance for visas, lodging, and local transportation
Flexible Scheduling to accommodate your time zone
Frequently asked questions
What are the surgical risks?
Bleeding, infection, and rare bladder or bowel injury—kept low by advanced minimally invasive techniques.
Will I need chemo or radiation?
Depends on stage and tumor grade; many early cases are managed with surgery alone.
Can I resume exercise?
Most patients return to low-impact activity within 6 weeks; full clearance by 3 months.
Ready to Take Control?
Discover how swift, personalized care in Valencia can fast-track your treatment and restore your peace of mind.
Request Consultation or Second Opinion

DOWNLOAD A FREE Roadmap
Download the Endometrial Cancer Roadmap (PDF)
Next Steps
More than a clinic — we are your international partner in healing.
With virtual consults, fast-track scheduling, and full travel support, we make Valencia endometrial cancer surgery seamless — wherever you live.