Can endometrial ablation cause cancer? Learn what research says, potential risks, symptoms to watch for, and when to consult your doctor.
Introduction
Can endometrial ablation cause cancer? This is a common and important question for women considering or who have already undergone this procedure. Endometrial ablation is widely used to treat heavy menstrual bleeding by destroying the lining of the uterus, offering relief without the need for major surgery. However, concerns have been raised about whether altering the uterine lining could increase the risk of developing endometrial or other gynecologic cancers.
Understanding the relationship between endometrial ablation and cancer risk requires looking at medical research, expert opinions, and post-procedure monitoring guidelines. While the procedure itself is not considered a direct cause of cancer, it may affect how symptoms are detected or how future conditions are diagnosed. This article explores the scientific evidence, potential risks, and what women should know to make informed, confident healthcare decisions.
Table of Contents
What is Endometrial Ablation?
Endometrial ablation is a minimally invasive gynecological procedure designed to reduce or stop heavy menstrual bleeding by destroying (ablating) the endometrium—the lining of the uterus. It is typically recommended for women who experience excessive or prolonged periods that have not improved with medication and who do not plan to become pregnant in the future.
The procedure works by targeting the uterine lining using controlled energy sources such as heat, cold, radiofrequency, or microwave energy. By removing or damaging this lining, menstrual flow is significantly reduced, and in some cases, periods may stop altogether. Endometrial ablation is usually performed as an outpatient procedure and does not require major surgery or large incisions.
There are several techniques used for endometrial ablation, including thermal balloon therapy, radiofrequency ablation, cryoablation (freezing), and heated fluid methods. The choice of method depends on factors such as uterine size and shape, medical history, and the provider’s expertise. Most procedures take less than an hour, and recovery time is generally short, allowing patients to return to normal activities within a few days.
While endometrial ablation can be highly effective for managing heavy bleeding, it is not a treatment for underlying conditions such as uterine cancer. Pregnancy after the procedure is rare but risky, which is why reliable contraception is recommended afterward. Understanding what endometrial ablation is—and what it is not—helps patients make informed decisions and set realistic expectations about outcomes and long-term care.
Can Endometrial Ablation Cause Cancer?
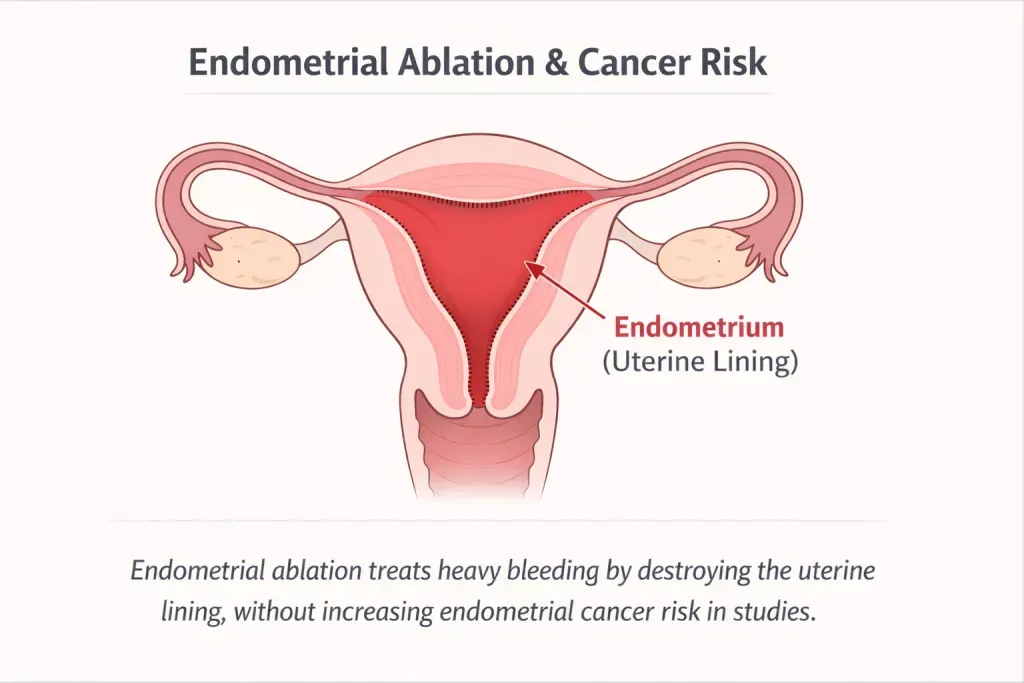
Based on the best available medical evidence, endometrial ablation does not cause cancer. Research consistently shows that women who undergo endometrial ablation do not have a higher risk of developing endometrial (uterine) cancer compared with women managed using other treatments for heavy menstrual bleeding.
What Studies Show About Cancer Risk?
Large population-based studies have compared women who had endometrial ablation with similar women treated using medical therapy or other non-ablative approaches. These studies found no increased rate of endometrial cancer in the ablation group versus comparison groups.
Importantly, researchers also examined whether cancer was being diagnosed later or at more advanced stages after ablation. The evidence shows that diagnosis timing and cancer stage were not worse in women who had undergone the procedure. In other words, endometrial ablation did not appear to hide cancer or lead to delayed detection at a population level.
What Systematic Reviews Conclude?
Systematic reviews, which analyze and synthesize results from multiple studies, reach the same overall conclusion. Across the available literature, endometrial ablation is not associated with an increased likelihood of developing endometrial cancer.
These reviews also conclude that prior ablation is generally not linked to delayed diagnosis when cancer does occur. While individual cases may require additional diagnostic steps due to post-ablation scarring, the overall evidence does not show a meaningful or consistent delay in identifying endometrial cancer.
Why People Think It Might Cause Cancer (Common Confusions)?
The belief that endometrial ablation may cause cancer does not come from scientific evidence, but from a few common misunderstandings about what happens after the procedure.
When endometrial cancer is discovered months or years after an ablation, many people assume the procedure must have caused it. In reality, this is a post hoc assumption—cancer was already developing independently due to existing risk factors, and the timing makes it appear related. Medical studies consistently show that ablation does not initiate cancerous changes in the uterus.
Endometrial ablation is designed to reduce or stop menstrual bleeding. Because abnormal bleeding is a well-known early symptom of endometrial cancer, people worry that cancer might be “missed” if bleeding no longer occurs. While bleeding patterns may change, cancer that develops after ablation still tends to produce symptoms—such as new bleeding, pelvic pain, or abnormal discharge—that prompt medical evaluation.
The procedure may cause scarring within the uterine cavity. In a small number of patients, this can make endometrial sampling or biopsy technically more difficult. However, this does not prevent diagnosis. Doctors can use ultrasound, hysteroscopy, or alternative diagnostic methods when needed. The need for additional testing is sometimes mistaken for delayed diagnosis, reinforcing the misconception that ablation causes cancer.
In short, these concerns arise from timing, symptom changes, and diagnostic complexity—not from evidence of increased cancer risk. When proper screening is done before ablation and symptoms are evaluated afterward, endometrial cancer can still be detected effectively.
Who Is at Higher Risk of Endometrial Cancer (Ablation or Not)
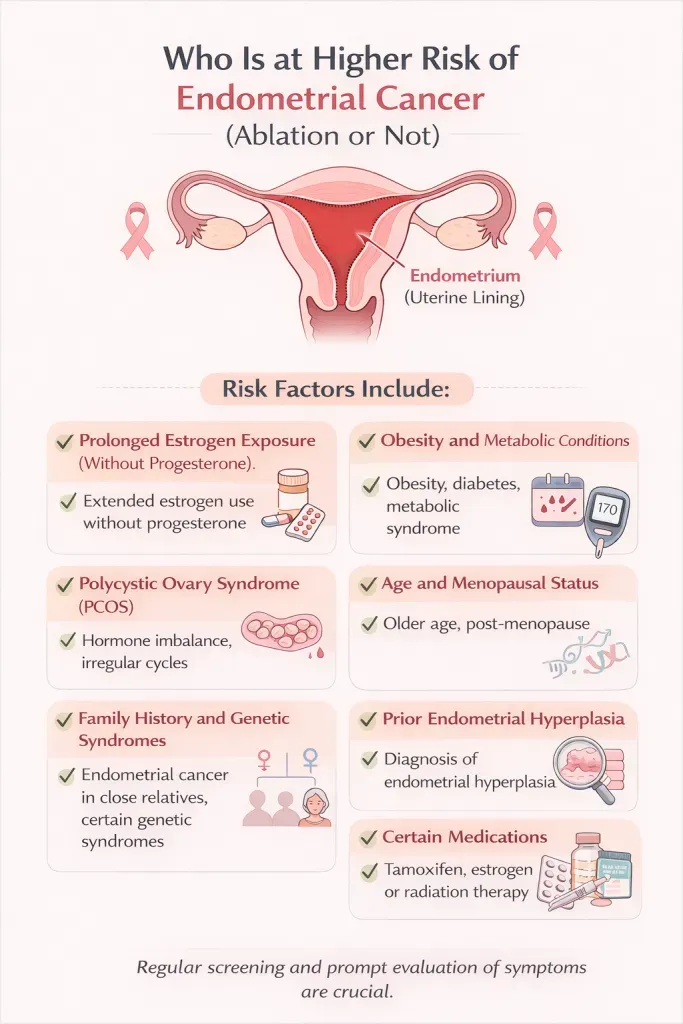
Endometrial cancer risk is driven by hormonal, metabolic, genetic, and age-related factors—not by whether someone has had endometrial ablation. Understanding these risks is important for everyone, regardless of treatment choice for heavy menstrual bleeding.
Prolonged Estrogen Exposure (Without Progesterone)
Anything that increases lifetime exposure to estrogen without adequate progesterone raises risk. This includes:
- Early onset of menstruation or late menopause
- Chronic anovulation (not ovulating regularly)
- Long-term estrogen-only hormone therapy
Estrogen stimulates the uterine lining; without progesterone to counterbalance it, abnormal cell growth is more likely.
Obesity and Metabolic Conditions
Excess body fat converts other hormones into estrogen, increasing circulating estrogen levels. Risk is higher in people with:
- Obesity
- Type 2 diabetes
- Metabolic syndrome
These factors are among the strongest predictors of endometrial cancer risk.
Polycystic Ovary Syndrome (PCOS)
PCOS often involves irregular ovulation and prolonged estrogen exposure. Without regular progesterone influence, the endometrium may thicken abnormally over time, increasing cancer risk if not properly managed.
Age and Menopausal Status
Risk rises with age, particularly after menopause. Any postmenopausal bleeding—whether light spotting or heavier flow—should always be evaluated, regardless of prior procedures like ablation.
Family History and Genetic Syndromes
A family history of endometrial or colorectal cancer can increase risk. People with hereditary cancer syndromes (such as Lynch syndrome) face a substantially higher lifetime risk and often require enhanced screening or preventive strategies.
Prior Endometrial Hyperplasia
Endometrial hyperplasia—especially atypical hyperplasia—is a known precursor to cancer. Individuals with a history of this condition remain at higher risk and need ongoing monitoring.
Certain Medications
Long-term use of medications that affect estrogen pathways (for example, tamoxifen) can increase endometrial cancer risk and warrants regular gynecologic follow-up.
Safety Checks Before Ablation (Critical Section)
Endometrial ablation can be a safe and effective treatment for heavy menstrual bleeding—but only when proper safety checks are completed beforehand. These evaluations are critical to rule out serious conditions, especially endometrial cancer or precancerous changes, and to ensure the procedure is appropriate for the patient.
Rule Out Endometrial Cancer and Precancer
Before ablation, the uterine lining must be assessed to confirm there is no endometrial cancer or atypical hyperplasia. This is typically done with an endometrial biopsy, which samples tissue from the uterine lining. Ablation should never be performed if cancer or precancer is present, as the procedure is not a treatment for malignancy.
Assess Uterine Structure and Lining Thickness
A transvaginal ultrasound is commonly used to evaluate uterine size, shape, and endometrial thickness. This helps identify fibroids, polyps, congenital abnormalities, or other structural issues that could affect both safety and effectiveness of the procedure.
Review Risk Factors and Medical History
A thorough review of personal risk factors is essential. This includes:
- Age and menopausal status
- Obesity, diabetes, or PCOS
- History of abnormal uterine bleeding patterns
- Family history of gynecologic or colorectal cancer
- Use of hormone therapy or medications affecting estrogen
Patients with higher baseline cancer risk may need additional evaluation or may be better suited to alternative treatments.
Confirm No Desire for Future Pregnancy
Pregnancy after endometrial ablation is uncommon but dangerous. Providers must confirm that the patient does not plan future pregnancies and discuss reliable contraception or permanent sterilization options if appropriate.
Evaluate for Active Infection or Other Contraindications
Active pelvic infection, uterine abnormalities that prevent safe device placement, or recent pregnancy are contraindications to ablation. Identifying these issues beforehand prevents complications.
FAQ’s
Can you get endometrial cancer after an ablation?
Across 11 analyzed studies, the reported incidence of endometrial cancer in women with prior endometrial ablation ranged between 0.0% and 1.6%. A total of 38 post-ablation cancer cases have been documented, with vaginal bleeding identified as the initial symptom in approximately 71% of patients.
Can endometrial ablation hide cancer symptoms?
Endometrial ablation does not cause cancer, but it may change typical warning symptoms, especially abnormal bleeding. Because many women have lighter or no periods after ablation, bleeding-related symptoms of endometrial cancer can be less obvious. This is why new or unusual symptoms after ablation should always be evaluated by a healthcare provider.
What symptoms after endometrial ablation should I worry about?
You should contact a doctor if you experience:
Bleeding that returns after a long period without bleeding
Any postmenopausal bleeding
Persistent pelvic pain or pressure
Unusual vaginal discharge
Worsening cramps months or years after ablation
These symptoms do not mean cancer is present, but they require medical evaluation.
Do doctors test for cancer before doing an endometrial ablation?
Yes. Before endometrial ablation, doctors are required to rule out endometrial cancer or precancerous conditions. This usually includes reviewing bleeding history and, when appropriate, performing tests such as an endometrial biopsy or imaging studies. Ablation should not be performed if abnormal uterine bleeding has not been properly evaluated.
Can you still get an endometrial biopsy after ablation?
Yes, but it can be more challenging in some cases. Scarring from ablation may make standard biopsy techniques harder, but doctors can often still evaluate the uterus using ultrasound, hysteroscopy, or dilation and curettage (D&C) if needed. Diagnostic options remain available after ablation.
Conclusion
Current medical evidence shows that endometrial ablation does not cause endometrial cancer. Studies and systematic reviews consistently find no increased cancer risk after the procedure, and cancers diagnosed later are usually linked to existing risk factors rather than ablation itself. While bleeding patterns may change after treatment, symptoms such as new bleeding or pelvic pain still prompt evaluation, making timely diagnosis possible when proper screening and follow-up are in place.