DISEASES
Uterine & Genital Prolapse: Restore Comfort & Confidence — Trusted by Women Worldwide
Dr. Lucas Minig — Expert in HIGH COMPLEX Pelvic Reconstructive Surgery

You deserve a life free from pelvic pressure
If you’re feeling a persistent heaviness or fullness in your pelvis, experiencing unexpected urinary leaks, or finding it hard to stay active, you may be dealing with uterine and/or genital prolapse. Everyday movements—lifting groceries, running, even coughing—can cause discomfort or trigger incontinence, leaving you hesitant to move freely.
When simple remedies no longer bring relief, it’s time for a personalized, expert approach.
Whether you’re based in Europe, North America, Latin America, or beyond, our Valencia center welcomes international patients seeking world-class care. Dr. Minig and his multidisciplinary team bring over 20 years of experience in advanced pelvic surgery, supported by conservative therapies, nutritional strategies, and mind–body practices to help you reclaim your confidence, comfort, and quality of life.
Our focus is clear: relief and improve your quality of life, offering world-class surgical outcomes with a truly human approach.
Request Internacional Second Opinion

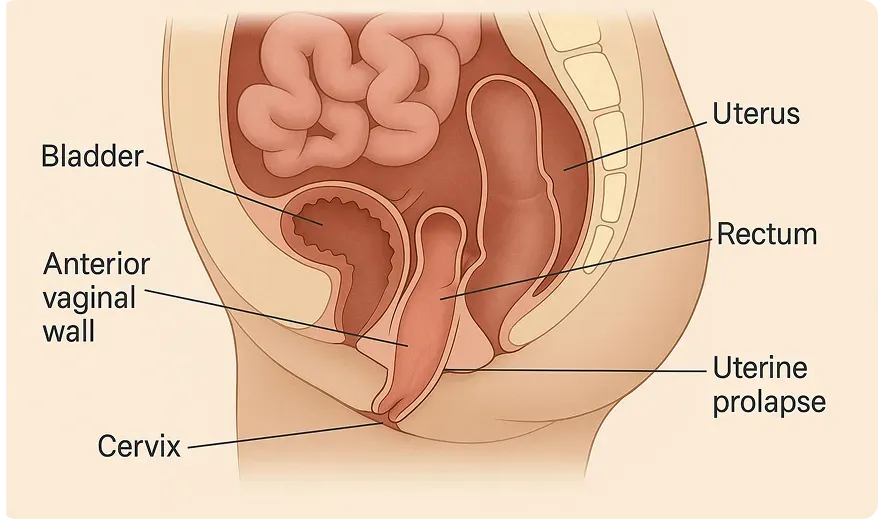
What is uterine & genital prolapse?
Uterine (or genital) prolapse occurs when the pelvic floor muscles and ligaments weaken, allowing the uterus and / OR the bladder or rectum—to descend into the vaginal canal. This can lead to:
- A visible or palpable bulge at your vaginal opening
- A constant feeling of pressure or “something falling out”
Recognize the symptoms early
Key factors include:
Early intervention broadens your options. Watch for:
- Pelvic Heaviness or Fullness
- Urinary Incontinence (cough, laugh, exercises)
- Frequent Urination or Incomplete Emptying
- Discomfort During Intercourse
- Back or Groin Pain
- Vaginal Bulge or Tissue Protrusion
Why it happens & who’s at risk
Uterine prolapse most commonly affects:
- Women After Vaginal Birth, especially multiple or traumatic deliveries
- Postmenopausal Women, due to decreased estrogen and connective-tissue strength
- Chronic Strainers (constipation, chronic cough)
- Heavy Lifters (occupational or recreational)
Other factors include obesity, prior pelvic surgery, connective-tissue disorders, and genetics.
DOWNLOAD A FREE GUIDE
Download the Prolapse Recovery & Exercise Guide (PDF)
How we diagnose fibroids—fast & clear
- Comprehensive Consultation
We review your history, symptom severity, and lifestyle goals. - Physical Examination
We assess pelvic support to determine the prolapse stage. - Urodynamic Testing (if urinary symptoms)
Measures bladder function to plan any combined incontinence repair. - Imaging When Needed
Ultrasound or MRI to evaluate supportive structures and rule out other causes.
Request Consultation or Second Opinion

Your personalized & multidisciplinary treatment pathway
We personalize every step — whether you are local or traveling from overseas.
Our team coordinates closely with international patients to minimize travel stays and ensure fast, streamlined care.
No two people—and no two diagnoses—are exactly the same. That’s why we take the time to understand your stage, your goals, and your vision for the future, including fertility and quality of life. You are not a case—you are a person. And your care plan will reflect that.
We never believe in “one-size-fits-all.” Your plan can include:
1. Conservative Therapies
- Pelvic-floor physical therapy (Physiotherapy, Rehabilitation)
- Vaginal pessaries (custom-fitted support devices)
- Estrogen therapy for postmenopausal tissue health
- Behavioral modifications (manage constipation, modify lifting techniques)
“Many women find significant relief—and postpone or even avoid surgery—with a structured conservative plan.”
2. Minimally Invasive Repair
- Laparoscopic Sacrocolpopexy or Robotic-Assisted Suspension Restores uterine support with mesh or sutures while preserving anatomy.
- Vaginal Hysteropexy (uterus-sparing)
- Colporrhaphy (anterior/posterior repair for bladder/rectum support)
- Combined Sling Repair for stress urinary incontinence
With over 95% of our repairs performed laparoscopically or robotically, you benefit from smaller incisions, less pain, and a quicker recovery.
Recovery & healing roadmap
What to Expect:
Days 1
Walking within hours post-surgery
Days 10–12
Home recovery with virtual follow-up; and direct access to Dr. Minig 24/7
Weeks 2–4
Normal activities resume according with level of pain; discomfort fades. Back to full routines, including exercise
Months 2–3
Back to full routines, including exercise
Ongoing
Annual ultrasounds help monitor for recurrence
Why choose Dr. Minig & our team
Extensive specialized oncology training in the main medical centers in Italy and the United States
- 20+ Years’ Expertise in pelvic reconstructive surgery
- Uterus-Preserving Focus: Over 99% of eligible patients keep their uterus
- Comprehensive Care: From conservative therapies to advanced minimally invasive surgical repair
- Global Reach: Personalized logistical support for international patients
- Industry-Leading Research & Innovation
“Dr. Minig’s expertise let me restart my workouts just two months after surgery—without fear of a bulge returning.”
— Marta S., Valencia

International patient welcome
Whether you’re in Europe, North America, or beyond, our clinic offers:
Tele-Consultations in English, Spanish and Italian
Concierge Travel Assistance for visas, lodging, and local transportation
Flexible Scheduling to accommodate your time zone
Frequently asked questions
Can I avoid surgery altogether?
Mild cases often improve with pelvic therapy and pessaries, but surgery offers the most definitive correction.
How long before I can resume exercise?
Most patients return to low-impact activities by 6 weeks; high-impact sports follow by 3 months post-op.
Will prolapse come back?
Recurrence rates are low (< 10%) with modern techniques and adherence to recovery protocols.
Next Steps
More than a clinic — we are your international partner in healing.
With virtual consults, fast-track scheduling, and full travel support, we make Valencia prolapse surgery seamless — wherever you live.